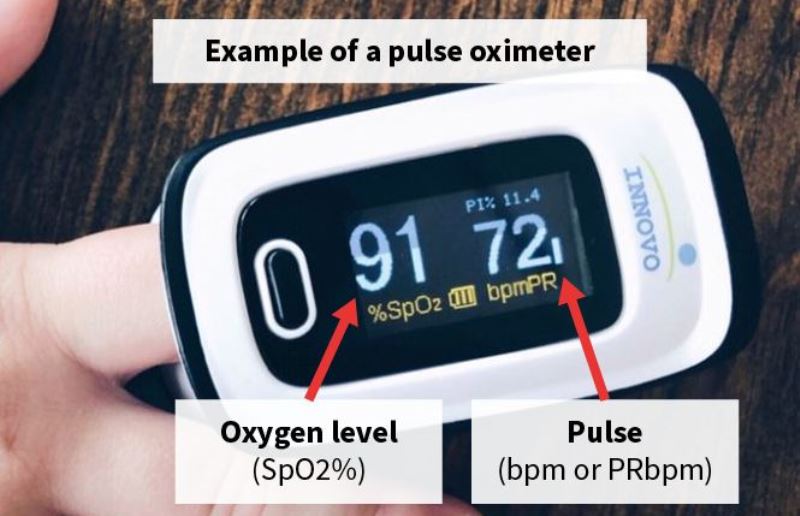
For most people, a normal pulse oximeter reading for their oxygen saturation level is between 95% and 100%.
If you have a lung disease like COPD or pneumonia, your normal oxygen saturation level may be lower. Your health care provider will let you know what levels are acceptable. Your oxygen saturation levels may also be lower if you live in an area with high elevation.
How to measure the oxygen level?
With a pulse oximeter, an oximeter uses two frequencies of light (red and infrared) to determine the percentage (%) of hemoglobin in the blood that is saturated with oxygen. The percentage is called the blood oxygen saturation or SpO2.
A pulse oximeter also measures and displays the pulse rate at the same time it measures the SpO2 level.
How is oxygen saturation measured?
Oxygen from the atmosphere reaches the lungs through respiration. Each lung contains nearly 300 million alveoli that are surrounded by blood capillaries. Since the alveolar and capillary walls are very thin, the oxygen that passes into the alveoli is immediately transferred to the blood capillaries.
Typically in adults, the transfer would take about 0.25 seconds at rest.
A large proportion of the oxygen that diffuses into the blood binds to the hemoglobin in the red blood cells, while a portion of the oxygen dissolves in the blood plasma.
Oxygen-enriched blood (arterial blood) flows through the pulmonary veins, then to the left atrium and left ventricle, and finally to the body’s organs and cells.
The amount of oxygen carried by the body is determined primarily by the degree to which hemoglobin binds oxygen (pulmonary factor), the concentration of hemoglobin (anemic factor), and cardiac output (cardiac factor).
Oxygen saturation is an indicator of oxygen transport in the body and indicates whether enough oxygen is being supplied to the body, especially the lungs.
The pulse oximeter can also measure the pulse rate. The volume of blood pumped by the heart per minute is called the cardiac output. The rate of pumping for one minute is called the pulse rate. These indicators of cardiac function can be determined by the pulse oximeter.
How does oxygen get into your body?
We need oxygen to sustain our lives. Oxygen from the atmosphere reaches the lungs through respiration and the blood through the pulmonary capillaries. It is then carried throughout the body by the blood.
- Oxygen is inhaled into the lungs and carbon (carbon dioxide) is exhaled from the lungs into the air. This process is called ventilation.
- Inhaled air flows into the upper airways, then into the peripheral airways, and is finally distributed to the lungs. This process is called distribution.
The lungs consist of tissues called alveoli. Oxygen is absorbed from the alveoli, then into the lung capillaries via alveolar membranes, while carbon dioxide moves from the lung capillaries to the alveoli. This process is called diffusion.
How does oxygen get into the blood?
One of the main functions of the blood is to receive oxygen from the lungs and transport it to the tissues of the body. At the same time, the blood receives carbon dioxide from the tissues and returns it to the lungs.
The amount of gas dissolved in a liquid (blood, in this case) is proportional to the pressure (partial pressure) of the gas.
Also, each gas has a different solubility. Only about 0.3 ml of gaseous oxygen dissolves in 100 ml of blood per mmHg (pressure).
This amount is only 1/20 of the solubility of carbon dioxide. This suggests that a human being would not be able to get enough oxygen if solubility was the only way to get oxygen in the blood.
For this reason, hemoglobin (Hb) has an important role as an oxygen carrier. One molecule of hemoglobin can bind 4 molecules of oxygen, and 1 g of hemoglobin can bind 1.39 ml of oxygen.
Since 100 ml of blood contains approximately 15 g of hemoglobin, the hemoglobin contained in 100 ml of blood can bind 20.4 ml of oxygen.
Hemoglobin saturation
What is oxygen saturation?
Hemoglobin bound to oxygen is called oxygenated hemoglobin (HbO2). Hemoglobin not bound to oxygen is called deoxygenated hemoglobin (Hb).
- Oxygen saturation is the ratio of the oxygenated hemoglobin to the hemoglobin in the blood, as defined by the following equation:
- Oxygen saturation = C (HbO2) / C (HbO2)+C (Hb) x 100 (%)
- C (Hb) = Concentration of deoxygenated hemoglobin
- C (HbO2) = Concentration of oxygenated hemoglobin
Oxygen saturation can be assessed by SaO2 or SpO2. SaO2 is the oxygen saturation of arterial blood, while SpO2 is the oxygen saturation detected by the pulse oximeter. They are called arterial blood oxygen saturation and percutaneous oxygen saturation.
How to calculate PaO2 from SpO2?
Does the ratio of PaO2 to SpO2 always remain the same?
The amount of dissolved oxygen in the blood is proportional to the partial pressure of oxygen.
The amount of oxygen bound to hemoglobin will increase as the partial pressure of oxygen increases. The partial pressure of oxygen is expressed as PO2 and the partial pressure of arterial blood is expressed as PaO2.
In contrast, the amount of oxygen bound to hemoglobin does not increase in proportion to the partial pressure of oxygen. The increase may be indicated by an S-shaped curve as shown in the graph below. This is called the oxygen dissociation curve.
The oxygen dissociation curve is called the “oxygen dissociation standard curve” where body temperature is 37°C, pH 7.4
The curve may shift to the right or left, depending on patient conditions.
If the body temperature decreases and pH increases, the curve will shift to the left. If the temperature increases and pH decreases, the curve will shift to the right.
for what purpose is oximeter used
Pulse oximeters were first used to monitor vital signs during operations and anesthesia.
Since the device is non-invasive and allows for immediate, real-time monitoring, its use has been expanded to include other purposes such as screening, diagnosis, patient monitoring, and self-monitoring. Below are examples of how the pulse oximeter is used.
The severity of a disease
Determining the severity of disease: The severity of a disease can be determined by clinical symptoms including SpO2.
Blood gas analysis
Deciding whether to perform blood gas analysis in order to better understand the patient’s condition.
Hospitalization of patients
Deciding on hospitalization of patients with chronic diseases when in the acute phase. The need for hospitalization is determined by clinical symptoms including SpO2.
Non-invasive ventilation
Starting Noninvasive Positive Pressure Ventilation (NPPV) for patients with chronic respiratory failure.
For patients with restrictive ventilation disorders (such as late-stage symptoms of pulmonary tuberculosis, or kyphoscoliosis), those in a mild phase of COPD, obesity hypoventilation syndrome, CSR, acute phase of COPD, neuromuscular disorder, etc.
Vital sign monitoring
Vital sign monitoring of hospitalized patients. SpO2 is the fifth most important vital sign after pulse rate, body temperature, blood pressure, and respiration. Even if no respiratory symptoms are observed, the level of SpO2 should be recorded.
If treatments or examinations influence a patient’s respiration, their respiratory condition should be followed up as appropriate.
In respiratory and cardiovascular wards, routine SpO2 monitoring is performed by nurses on each patient during their rounds in the morning, afternoon and evening.
Management of patients
Daily management of HOT patients with chronic respiratory failure. A growing number of HOT patients with chronic respiratory failure have used the pulse oximeter for routine monitoring.
Sleep apnea syndrome.
Screening for sleep apnea syndrome. A pulse oximeter with memory function is used to record oxygen saturation (SpO2) during sleep to determine the frequency of hypoxemia events (oxygen desaturation index), as well as the duration of desaturation.
Dysphagia symptoms
Screening for dysphagia and its monitoring by examination. The pulse oximeter is used as a part of monitoring patients with dysphagia when they are observed while eating.
Diagnosis of polycythemia
The oxygen saturation may decrease in patients with pulmonary diseases such as COPD, sleep apnea syndrome, cardiac disorders such as valvulopathy, as well as persons living at high altitudes. In these cases, the bone marrow is stimulated to produce more red blood cells and consequently polycythemia (secondary polycythemia). The pulse oximeter may be used to measure SpO2 and determine the causes of polycythemia.
Monitoring during examinations
The pulse oximeter is an essential device for bronchoscopy. Prior to examinations, sedatives are administered. Patient conditions are observed by monitoring changes in heart rate and SpO2 in order to ensure safe examinations. The pulse oximeter is often used with photogastroscopy and fibroptic colonoscopy.
-Assessment and risk management of respiratory rehabilitation and exercise therapy

FDA approved pulse oximeter
The use of OTC oximeters has increased as a result of the pandemic.

Oxygen Machine for Home Use
Everyone has different reasons for wanting to upgrade to the convenience of a portable oxygen concentrator. But typically it’s for one of the following reasons.

What happens when your Oxygen Level drops to 70?
If you have wondered: How to restore oxygen levels in patients?

How to increase Blood Oxygen Level?
A low level of oxygen in the blood, in addition to revealing the presence of possible lung disease.

Average Oxygen Level
What are average readings? A normal oxygen level is usually 95% or more.