Body temperature measurement with medical devices in today’s pandemic environment encompasses a wide variety of needs and applications.
To meet this wide range of needs, the industry has developed a large number of sensors and devices to handle this demand.
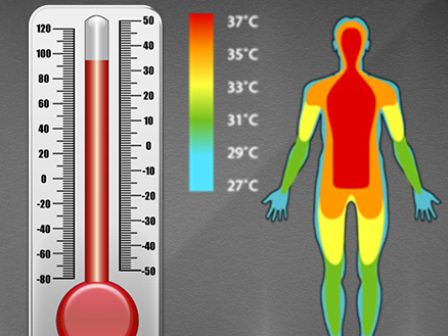
To understand the human body, a healthy body maintains its normal temperature within a narrow range, using thermoregulatory mechanisms. Extremes of temperature are easier to interpret.
At 43 ° C or higher, cells are irreparably damaged, putting your life in danger. On the contrary, as the temperature drops, cellular processes slow down and the metabolic rate drops; this suggests that consciousness is lost 33 ° C.
The body is generally more tolerant of lower than high temperatures.
Temperature measurement device
Body temperature represents the balance between heat production and heat loss. If the rate of heat generated equates to the rate of heat loss, the core body temperature will be stable.
All metabolizing body cells manufacture heat in varying amounts. Therefore, body temperature is not evenly distributed across the body.
Core body temperature is found in the blood supplying organs such as the brain and those in the abdominal and thoracic cavities. The core temperature may be affected by intrinsic factors and, to a lesser degree, extrinsic (environmental) factors.
Peripheral temperature is recorded in tissues such as the skin, where environmental factors and a lack of insulating connective tissue influence temperature.
A healthy body maintains its temperature within a narrow range using homeostatic thermoregulation mechanisms. The normal range for core temperature in the literature varies, although 36° C – 37.5° C is acceptable in clinical practice.

Instrument used to measure Normal body temperature
The normal core temperature range varies, although 36 ° C – 37.5 ° C is acceptable in clinical practice.
It is estimated that with every 1 ° C increase in body temperature there is a 10% increase in the rate of enzyme-controlled chemical reactions.
At 43 ° C or higher, cells are irreparably damaged, putting your life in danger. On the contrary, as the temperature drops, cellular processes slow down and the metabolic rate drops; this suggests that consciousness is lost 33 ° C.
The body is generally more tolerant of lower than high temperatures.
Importance of taking body temperature
Why is thermoregulation important? There are many clinical indications for measuring body temperature, including:
- To obtain a reference temperature that allows comparisons with future temperatures.
- Observe and monitor patients for changes that indicate infection.
- Monitor the effectiveness of antimicrobial therapy treatment for infections.
- Before and during a blood transfusion to monitor for signs of a possible reaction.
Measuring body temperature
The measurement of core body temperature may seem simple, but several issues affect the accuracy of the reading. These include the measurement site, the reliability of the instrument, and user technique.
Practitioners must understand the advantages and disadvantages associated with the chosen method so they can explain the procedure to patients and obtain valid consent.
True core temperature readings can only be measured by invasive means, such as placing a temperature probe into the oesophagus, pulmonary artery, or urinary bladder.
It is not practical, nor indeed necessary, to use such sites and methods in all cases; they tend to be reserved for patients who are critically ill.
Non-invasive sites such as the rectum, oral cavity, axilla, temporal artery (forehead), and external auditory canal are accessible and are believed to provide the best estimation of the core temperature.
The temperature measured between these sites can vary greatly, so the same site ought to be used consistently and recorded on the chart with the reading.

Body temperature chart
Body temperature should be measured and recorded regularly with precision, consistency, and diligence. Practitioners should be acutely aware of patients’ temperature because it serves as a useful indicator of change in their clinical condition
A review has illustrated that none of the methods for measuring the temperature at the bedside is perfect. Once a site and a method have been selected, they must be used consistently to ensure accuracy and patient safety.
List of instruments used to measure temperature
The instruments used to measure body temperature are medical thermometers, body temperature is a vital sign and it is important to measure it accurately. This article reviews and compares the various methods available to measure temperature accurately and quickly.
- Body Temperature Measurement Devices:
- Forehead Thermometer
- Tympanic thermometer
- Digital oral thermometer
- Digital axillary thermometer
- Digital rectal thermometer
- Digital basal thermometer
- Baby pacifier thermometer
- Skin temperature thermometer
Forehead Thermometer
Temporal artery temperature: The temporal artery thermometer is quick to use. It is held over the forehead and senses infrared emissions radiating from the skin. However, its reliability and validity have not been widely tested.
A single-center study comparing it with other methods found that, despite the infection control advantages of this non-touch method, it underestimated body temperature compared with the control.
Tympanic thermometer
Tympanic temperature: The tympanic thermometer senses reflected infrared emissions from the tympanic membrane through a probe placed in the external auditory canal. This method is quick (<1 minute), minimally invasive, and easy to perform.
It has been reported to estimate rapid fluctuations in core temperature accurately because the tympanic membrane is close to the hypothalamus.
Although its accuracy and reliability have been questioned in many studies in the past decade, with differing outcomes, tympanic thermometry continues to be used. Operator error and poor technique are frequently cited problems, so training is recommended.
Ear wax is known to reduce the accuracy of readings, so it is recommended that the ear be inspected before measurement.
Digital oral thermometer
The oral cavity temperature is considered to be reliable when the thermometer is placed posteriorly into the sublingual pocket. This landmark is close to the sublingual artery, so this site tracks changes in core body temperature.
Electronic or disposable chemical thermometers may be used. Low-reading thermometers may be of some use. Mercury in glass-thermometers can no longer be bought because of European Council rules.
Care must be taken to avoid the anterior region immediately posterior to the lower incisors because the temperature here is substantially lower.
Factors affecting accuracy include recent ingestion of food or fluid, having a respiratory rate >18 per minute, and smoking.
The advantages of this site are that the measurement does not appear to be influenced by oral fluids or diet, environmental temperature, or other extraneous variables. If patients have been lying with their ear on a pillow, allow 20 minutes to elapse so the temperature can normalize.
Digital axillary thermometer
Axillary temperature: Temperature is measured at the axilla by placing the thermometer in the central position and adducting the arm close to the chest wall.
The literature suggests that this is an unreliable site for estimating core body temperature because there are no main blood vessels around this area, electronic digital thermometers can be used on this site as a reliable alternative in older people.
Digital rectal thermometer
Rectal temperature is said to be the most accurate method for measuring the core temperature. However, obtaining this is more time-consuming than other methods and might be considered unfavorable for some patients. Practitioners should pay particular attention to issues of privacy.
The presence of feces prevents the thermometer from touching the wall of the bowel and may generate inaccurate readings. This method does not track immediate changes to core temperature because of the low flow of blood to the area, so core temperature may be under-or overestimated at times of rapid flux.
Digital basal thermometer
A basal thermometer is used by women to track ovulation through changes in temperature. It is an extremely sensitive thermometer that records temperatures to 0.1 degrees Fahrenheit increments, rather than 0.2 degrees Fahrenheit increments.
Baby pacifier thermometer
Another option for young children is the pacifier thermometer. This thermometer is shaped like a pacifier and after your child sucks on it for about 90 seconds, an oral temperature is taken.
Skin temperature thermometer
Chemical thermometers can be applied to the forehead or axilla, and the temperature is read to the nearest 1°C based on color change. Some thermometers display the actual temperature, but others contain an offset, and therefore, display the estimated core temperature.
Sensitivity for detecting fever was close to 90% in some studies, but it was as low as 30% in others, with rectal temperatures being the reference standard. Ambient temperature can affect measurements.
The most read
What instrument is used for measuring body temperature?
Most people would say that thermometers measure temperature, and that is true, but there are many different types. Also, some things are too small to use a standard bulb thermometer to determine your body temperature.
Normal Body Temperature
Your body has an internal thermostat and your goal is to keep your temperature as close to your goal as possible. What’s the normal body temperature?

Medical Grade Thermometer
As people plan to get back into a rut, many are considering buying technologies that can detect elevated temperatures.

Infrared Thermometer Price
A home use infrared thermometer is a medical device intended for users in any environment outside of a professional healthcare facility.

What is a Normal Forehead Temperature?
What is a “normal” human body temperature? That question is a bit more difficult to answer than you think.